Varicose Veins vs. Spider Veins: Understanding the Differences
Varicose veins and spider veins are common venous conditions that affect many people. Although they may look similar at first glance, these two types of veins have distinct characteristics, causes, and treatment approaches. Understanding the differences and knowing when to seek medical advice can help you protect your vein health and prevent complications. In this article, we explore what sets varicose veins and spider veins apart, their symptoms, risk factors, prevention strategies, and treatment options.
What Are Varicose Veins?
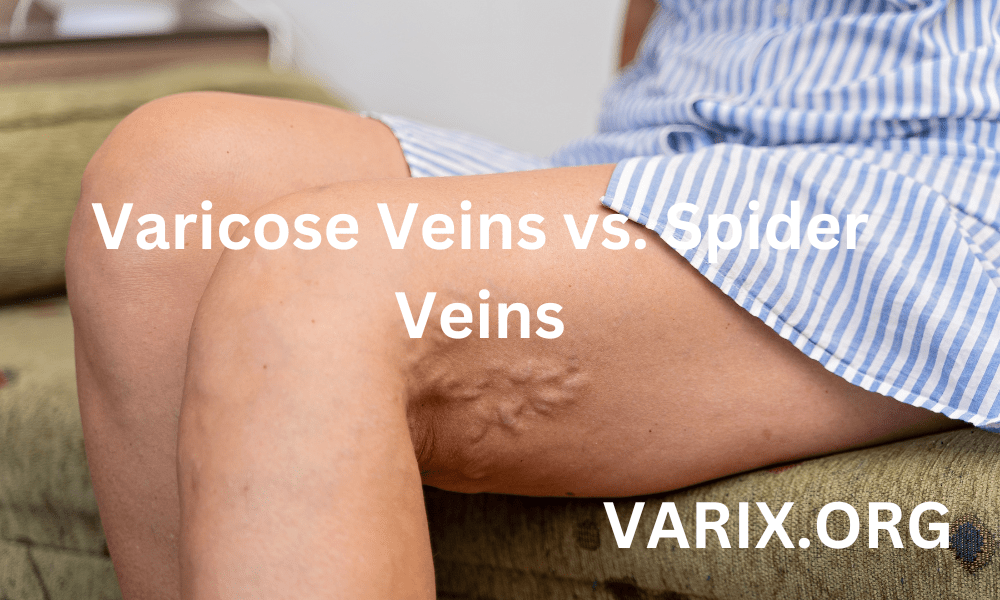
Varicose veins appear as enlarged, swollen, and twisted veins that protrude above the skin surface. They typically develop in the legs and feet, where increased pressure from standing and walking forces blood through weakened valves. When these valves fail to close properly, blood flows backward and pools in the veins, causing them to stretch and become visible. Varicose veins can range in color from dark blue to purple and may appear bulging or cord-like.
Causes of Varicose Veins
- Valve Malfunction: Vein valves weaken or become damaged, allowing blood to flow backward and pool.
- Increased Blood Volume: Hormonal changes, especially during pregnancy, increase blood volume and pressure on leg veins.
- Age: As you get older, vein walls lose elasticity and valves weaken.
- Genetics: A family history of varicose veins raises your risk.
- Occupational Factors: Jobs requiring long periods of standing or sitting can impede blood flow and contribute to varicosities.
- Obesity: Excess weight adds pressure on leg veins, impairing circulation.
Symptoms of Varicose Veins
- Aching or heaviness in the legs, especially after prolonged standing.
- Swelling and fluid retention in the ankles and feet.
- Itching or burning sensation around the affected veins.
- Visible, bulging veins that are raised above the skin surface.
- Skin discoloration or ulcers near the ankles in severe cases.
What Are Spider Veins?
Spider veins are smaller, dilated blood vessels that appear close to the surface of the skin. They often show a web-like pattern of red, blue, or purple lines that resemble a spider’s web—hence the name. Spider veins usually occur on the legs and face but can develop on other body parts. Unlike varicose veins, spider veins are typically painless and are most often a cosmetic concern. However, in some cases, they can cause mild itching or discomfort.
Causes of Spider Veins
- Increased Pressure: Similar to varicose veins, spider veins result from pressure on small blood vessels, often due to standing or sitting for extended periods.
- Hormonal Factors: Hormone fluctuations during puberty, pregnancy, and menopause can weaken capillary walls, leading to spider veins.
- Sun Exposure: UV rays can damage skin and superficial blood vessels, especially on the face.
- Genetics: A family history of spider veins increases susceptibility.
- Skin Trauma: Injuries or skin inflammation can lead to broken capillaries and spider veins.
Symptoms of Spider Veins
- Thin, branching lines of red, blue, or purple close to the skin surface.
- Mild itching or burning in the affected area in rare cases.
- Often asymptomatic, but can cause minor discomfort for some individuals.
Varicose Veins vs. Spider Veins: Key Differences
Although varicose veins and spider veins both relate to faulty veins, several factors distinguish them. Understanding these distinctions can help you identify which condition you have and choose the most appropriate prevention or treatment plan.
| Feature | Varicose Veins | Spider Veins |
|---|---|---|
| Appearance | Large, bulging, twisted, and rope-like veins | Small, thin, web-like clusters of red or blue lines |
| Size | Typically larger than 3 millimeters in diameter | Usually less than 1 millimeter in diameter |
| Depth | Located deeper below the skin surface | Very close to the skin surface |
| Symptoms | Aching, heaviness, swelling, itching, and risk of ulcers | Mostly a cosmetic concern; sometimes mild itching or burning |
| Health Impact | Can lead to complications like blood clots, ulcers, and deep vein thrombosis | Rarely leads to serious health issues, primarily cosmetic |
| Treatment Options | Compression stockings, sclerotherapy, laser therapy, surgery | Sclerotherapy, laser treatments, topical creams for cosmetic improvement |
Risk Factors for Both Conditions
Several factors increase the likelihood of developing either varicose veins or spider veins. Recognizing and addressing these risk factors can help prevent vein issues from worsening and promote overall vascular health.
- Age: Vein valves weaken over time, increasing risk.
- Genetics: Family history of venous conditions raises susceptibility.
- Hormonal Changes: Pregnancy, menopause, and hormone therapy can weaken vein walls.
- Prolonged Standing or Sitting: Jobs that require long hours in one position impede circulation.
- Obesity: Excess weight adds pressure on veins, impairing blood flow.
- Sedentary Lifestyle: Lack of regular exercise allows blood to pool in leg veins.
- Sun Exposure: UV damage can lead to broken capillaries on the face.
When to Seek Medical Advice
While spider veins are often harmless, varicose veins can lead to more serious complications if left untreated. It is important to consult a healthcare professional when you notice:
- Persistent leg pain, throbbing, or cramping that worsens after standing or sitting for long periods.
- Severe swelling or fluid retention in the legs or ankles.
- Skin changes such as discoloration, inflammation, or the development of ulcers near the veins.
- Signs of infection around a vein, including redness, warmth, or tenderness.
- Sudden, sharp pain, or swelling in one leg that may indicate a blood clot (deep vein thrombosis).
Prevention Strategies
Preventing vein issues involves adopting healthy habits that support proper circulation and reduce pressure on leg veins. Below are evidence-based strategies you can start implementing today.
- Stay Active: Engage in regular exercise such as walking, swimming, or cycling to promote blood flow and strengthen leg muscles.
- Maintain a Healthy Weight: Losing excess weight helps reduce pressure on leg veins and improves circulation.
- Wear Compression Stockings: These garments apply gentle pressure to leg veins, helping blood return to the heart more efficiently. Choose the correct compression level based on a healthcare provider’s recommendation.
- Elevate Your Legs: When resting, prop your legs on a pillow to raise them above heart level for 15 to 20 minutes several times a day to reduce swelling.
- Avoid Prolonged Sitting or Standing: If your job requires long periods in one position, take breaks every 30 minutes to walk, stretch, or do calf raises.
- Practice Good Posture: Avoid crossing your legs when sitting. Keep your feet flat on the floor or use a footrest to reduce venous pressure.
- Healthy Diet: Eat a balanced diet high in fiber, lean protein, fruits, and vegetables. Limit sodium to prevent fluid retention. Stay hydrated by drinking at least eight glasses of water a day.
Treatment Options
Treatment for varicose veins and spider veins depends on severity, symptoms, and cosmetic concerns. A healthcare professional can assess your condition and recommend the most appropriate approach.
Conservative and Home-Based Treatments
- Compression Stockings: Wearing graduated compression stockings daily helps improve circulation and reduce swelling.
- Leg Elevation: Elevate legs whenever possible to decrease vein pressure.
- Exercise: Low-impact activities such as walking, yoga, or swimming strengthen calf muscles and promote blood flow.
- Cold and Warm Compresses: Applying cold compresses reduces swelling, while warm compresses relax muscles and improve circulation.
- Massage: Gentle upward leg massages with a moisturizing lotion can stimulate blood flow and reduce discomfort.
Minimally Invasive Procedures
- Sclerotherapy: A solution is injected into the vein, causing it to collapse and fade over time. Effective for both varicose and spider veins.
- Endovenous Laser Therapy (EVLT): A laser fiber is inserted into the vein, delivering heat to close it off. Ideal for larger varicose veins.
- Radiofrequency Ablation (RFA): Radiofrequency energy is used to heat and seal the affected vein. Recovery time is typically shorter than surgery.
- Ambulatory Phlebectomy: Small incisions are made to remove varicose veins close to the skin’s surface. Local anesthesia is used, and downtime is minimal.
Surgical Treatments
- Vein Stripping and Ligation: Surgical removal of large varicose veins under general or spinal anesthesia. Steam treatments or ambulatory procedures may reduce recovery time.
- Endoscopic Vein Surgery: Used for severe cases where ulcers have formed. A small camera is inserted to visualize and close veins from the inside.
Recovery and Aftercare
Following treatment, proper aftercare is essential for optimal healing and to prevent recurrence. Strategies include:
- Continued Use of Compression Stockings: Wear them as directed by your provider for several weeks after treatment.
- Gradual Return to Activity: Avoid intense exercise for the first week; then resume low-impact activities and increase gradually.
- Follow-Up Appointments: Attend scheduled visits to monitor healing and ensure no complications such as infection or blood clots occur.
- Skin Care: Keep the treated area clean and moisturized. Protect skin from sun exposure with sunscreen to prevent pigmentation changes.
Conclusion
Varicose veins and spider veins are distinct conditions affecting your vein health. While spider veins are primarily a cosmetic concern, varicose veins can lead to discomfort and serious complications. By recognizing the differences, understanding risk factors, and implementing prevention strategies, you can reduce your chances of developing vein issues and maintain healthy circulation. If you notice concerning symptoms, consult a healthcare professional to explore treatment options tailored to your needs.
Early intervention and consistent self-care—such as wearing compression stockings, staying active, and elevating your legs—can go a long way in preventing vein problems from worsening. With the right combination of lifestyle modifications and medical treatments, you can enjoy improved vein health and overall well-being.
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The content provided should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional before making any decisions about your health or medical conditions. Never disregard or delay seeking professional medical advice due to the information provided in this article. The author and publisher of this article are not responsible or liable for any adverse outcomes resulting from the use or reliance on the information provided herein.